Patient Education

Rheumatology Consultation
What is Osteoporosis?
Rheumatology is a rapidly evolving medical sub-specialty, devoted to the diagnosis and therapy of rheumatic diseases. These diseases especially affect joints, tendons, ligaments, bones, and muscles. There are more than 200 types of these diseases, including rheumatoid arthritis, osteoarthritis, gout, lupus, back pain, osteoporosis, lupus and tendinitis. Some of these are very serious diseases that can be difficult to diagnose and treat. Rheumatic diseases can also involve internal organs.
The cause of every major rheumatological disorder is now best explained by imbalance in the autoimmune system. Hence, rheumatic diseases are often referred as autoimmune disease. The treatment modalities are also based on clinical research on autoimmune system. Evidence-based medical treatment of rheumatological disorders has helped patients with these disorders lead a near normal life.

Who Is a Rheumatologist?
A consultant rheumatologist is a doctor who specializes in diagnosing and treating arthritis and diseases related to rheumatology. Rheumatologists treat over 200 different health problems that affect the joints, bones, muscles and other internal organs (e.g. kidneys, lungs, blood vessels, brain). They focus on the non-surgical treatment of arthritis and related rheumatic diseases.
Rheumatologists treat arthritis, certain autoimmune diseases, vasculitis, musculoskeletal pain disorders, and osteoporosis. There are more than 200 types of these diseases, including rheumatoid arthritis, osteoarthritis, gout, lupus, back pain, osteoporosis, and tendinitis. Some of these are very serious diseases that can be difficult to diagnose and treat.
Adult rheumatologists are specifically trained to be highly skilled in:
1. Developing a differential diagnosis of rheumatic disorders and autoimmune diseases
2. Efficient use of diagnostic evaluations in rheumatic disorders
3. Selecting appropriate medical therapy for the treatment of rheumatic disease given the patient’s lifestyle and co-morbidities
4. Monitoring long-term efficacy and side effects of multiple medications including anti-inflammatory and biological agents used to treat rheumatic disease
5. Improving quality of life and decreasing disability of patients suffering from rheumatic disease
6. Providing longitudinal care for chronic rheumatic disease management such as rheumatoid arthritis, systemic lupus erythematosus and many more.)(should mention specific diseases or be more generic?)
7. Aspiration and injection of joints for diagnosis and treatment of rheumatic disease
8. Interpretation of radiographic, imaging, (e.g., ultrasound, MRI, CT, dual-energy X-ray absorptiometry) and laboratory studies in the context of rheumatic disease evaluation
9. Evaluation and management of osteoporosis
Rheumatologists provide a key role in the non-surgical treatment of osteoarthritis, soft tissue rheumatism, back pain, and other aspects of musculoskeletal health. Particularly, attention is paid to care of the geriatric patient who may be unable or does not wish to have extensive surgical procedures for the treatment of osteoarthritis, spinal stenosis as well as other conditions.
What causes rheumatic diseases?
Rheumatic diseases are an autoimmune conditions, which means it’s caused by the immune system attacking healthy body tissue. However, it’s not yet known what triggers this.
Your immune system normally makes antibodies that attack bacteria and viruses, helping to fight infection.
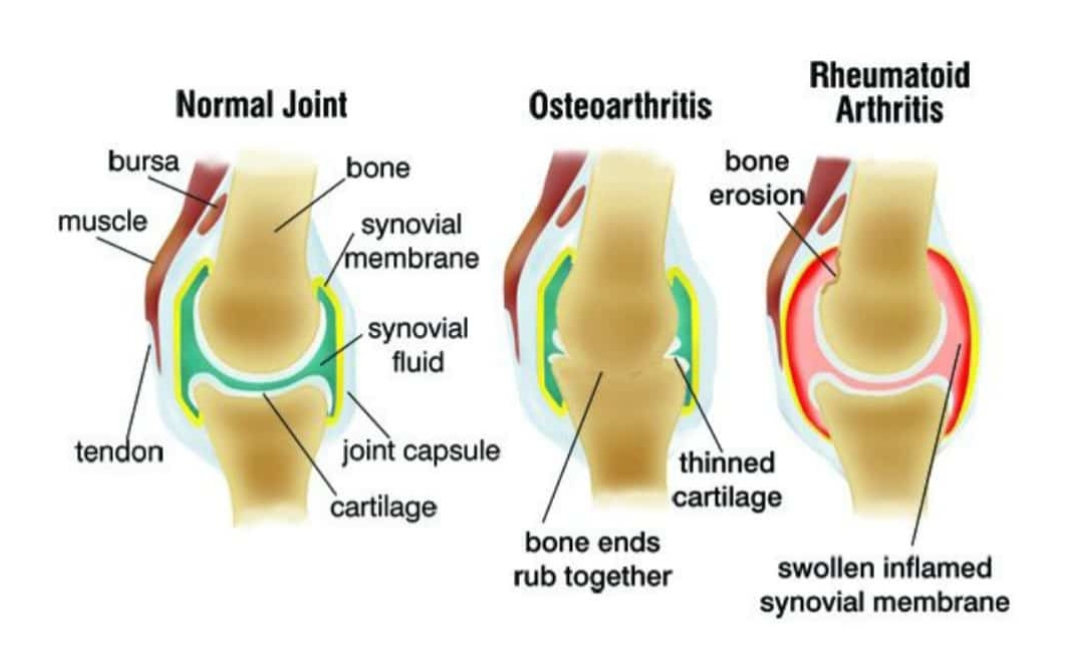
If you have rheumatic diseases, your immune system mistakenly sends antibodies to the lining of your joints, where they attack the tissue surrounding the joint.
This causes the thin layer of cells (synovium) covering your joints to become sore and inflamed, releasing chemicals that damage nearby:
- bones
- cartilage – the stretchy connective tissue between bones
- tendons – the tissue that connects bone to muscle
- ligaments – the tissue that connects bone and cartilage
If rheumatoid arthritis is not treated, these chemicals gradually cause the joint to lose its shape and alignment. Eventually, it can destroy the joint completely.
Various theories of why the immune system attacks the joints have been suggested, such as an infection being a trigger, but none of these theories has been proven.
Possible risk factors:—
you may be born with a susceptibility to a disease, but it may take something in your environment to get the disease started.
Some of these factors have been identified. For example, in osteoarthritis, inherited cartilage weakness or excessive stress on the joint from repeated injury may play a role. Certain viruses may trigger disease in genetically susceptible people. Gender is another factor in some rheumatic diseases. Lupus, rheumatoid arthritis, scleroderma, and fibromyalgia are more common among women. This indicates that hormones or other male-female differences may play a role in the development of these conditions.
There are several things that may increase your risk of developing rheumatoid arthritis, including:
- your genes – there’s some evidence that rheumatoid arthritis can run in families, although the risk of inheriting it is thought to be low as genes are only thought to play a small role in the condition
- hormones – rheumatoid arthritis is more common in women than men, which may be because of the effects of the hormone oestrogen, although this link has not been proven
- smoking – some evidence suggests that people who smoke have an increased risk of developing rheumatoid arthritis
Diseases Treated By Rheumatologist
- Rheumatoid arthritis
- Reactive Arthritis
- Psoriatic arthropathy
- Enteropathic spondylitis
- Juvenile idiopathic arthritis(JIA)
- Gout, pseudogout
- Septic arthritis
- Osteoarthritis
- Osteoporosis,osteomalacia
- Hypermobility syndrome
- Lupus
- Seleroderma(systmic selerosis)
- Dermatomyositis
- Polychondritis
- Vasculitis
- Microscopic polyangiitis
- Wegener’s granulomatosis
- Henoch-Schonlein purpura
- Takayasu’s arthritis
- Kawasaki’s disease
- Sjogren’s syndrome
- Polymyositis
- Polymyalgia rheumatiea
- Sarcoidosis
- Churg-Strauss Syndrome
Common Signs and Symptoms of Arthritis
- Swelling in one or more joints
- Stiffness around the joints in the early morning or with inactivity
- Constant or recurring pain or tenderness in a joint
- Difficulty using or moving a joint normally
- Warmth and redness in a joint
QUICK TEST TO ASSESS ARTHRITIS:
1} DO YOU HAVE EARLY MORNING STIFFNESS LASTING MORE THAN 30 MINUTES?
2} DO YOU GET PERSISTENT SWELLING OF ONE OR MORE JOINTS?
3} DO YOU GET PAIN ON SQUEEZING JOINTS?

Diseases For Patient Education
Do You Know?
While researchers suspect that some forms of arthritis have genetic links, having parents with arthritis does not necessarily mean that you will develop it. There are other triggers that can lead to arthritis, and the causes of many forms of arthritis are not fully understood
Speak to your doctor first to find out which forms of exercise will best suit your particular physical condition. Consider developing your exercise program with the help of a physical therapist or personal trainer skilled in working with people who have arthritis. Water exercises can be particularly effective for persons with joint conditions.
All drugs, even over-the-counter medications, have potential side effects, which you’ll find listed on the package or on an inserted sheet. You should be familiar with the information, and be aware of the side effects that require immediate medical attention. Your doctor or pharmacist can also provide more specific information about side effects based on your medical history and other medications you may be taking. Please contact your doctor or seek emergency treatment right away if you’re experiencing problems
There can sometimes be dangerous interactions between medications. Speak to your doctor about potential problems. Using your medical history and medication plan, they can quickly determine any potentially harmful interactions.
There are many alternative and complementary therapies. Some can be safe and effective, while others can be quite dangerous. We recommend that you speak to your doctor before trying any new treatment to determine safety and potential interactions with other medications you may be taking.
Although little evidence supports the benefit of chiropractic manipulation, acupuncture and herbal remedies for osteoarthritis, these may provide pain relief of an affected joint. It is important to communicate your use of complementary therapies with your healthcare provider to ensure that these treatments do not interfere with your other medical conditions or therapies.
We now know a great deal about what causes Rheumatic disesases and how to control it. While we cannot cure it at present, joint damage can now be prevented. This is achieved by the early implementation of disease-modifying antirheumatic drugs (DMARDs). These are essential to gain rapid control of the disease, in order to avoid joint erosions and long-term limitation of function.
Some patients with RA develop more generalized disease in which internal organs can be inflamed and damaged. This is quite rare, and rarer still today with our new therapies. Some of the patients who develop this problem have little nodules under the skin of their forearms. Internal problems can include:
Lung inflammation
Nerve irritation called neuropathy
Eye inflammation called scleritis
Dry eyes or dry mouth due to Sjogren’s syndrome
Each of these problems can be treated with many of the newer medications available for RA
Diet may play a role in some patients with RA. However, in most, a well-balanced diet is the correct prescription. Patients should keep a diary to determine whether eating one type of food is commonly associated with a flare of RA. If that is the case, a trial of avoiding that food is reasonable. Evidence is mounting to support achieving a healthy weight. Some studies suggest that eating fish two or more times per week is associated with less disease related symptoms.
Patients commonly report that stress, either physical or emotional, was present or severe when their RA began. This is true in other autoimmune disorders as well. Since the mind-body connection is real, most physicians appreciate the linkage between stress and disease onset or exacerbation. Because there are clear interactions between the nervous, immune and endocrine systems, the impact of stress on disease presentation and severity is explainable in physiologic terms. Obviously, life is stressful. Thus, how to employ stress reduction in a therapeutic regimen is up to the individual patient, in concert with the physician. Many patients have found benefits from mindfulness programs that facilitate learning tools to reduce the impact of stress.