Scleroderma
Scleroderma
What is Scleroderma?
An older name for systemic sclerosis is scleroderma, which means hard skin. Thickening and hardening of the skin is the most obvious symptom of systemic sclerosis but it can also affect the body’s internal organs. The word ‘systemic’ refers to a disease that can affect many differen organs in the body.
Systemic sclerosis can affect the joints, muscles, blood vessels and digestive system. It affects the lungs of about half the people with the condition, although this doesn’t always cause symptoms. It can also affect the kidneys, but this is rare
What are the different types of Scleroderma?
There are two main classes of Scleroderma.
- Localized Scleroderma affects only certain parts of the body [ skin & related structures].
- Systemic Scleroderma affects the whole body [affects the tissues beneath the skin such as the blood vessels & major organs].

What are the causes of Scleroderma?
Systemic sclerosis develops because of changes that occur in the body’s connective tissues. These tissues lie under the surface of the skin and also in and around the body’s internal organs and blood vessels.
Systemic sclerosis leads to too much fibrous connective tissue, which is similar to scars that form after an injury. Scar tissue contains a protein called collagen, which is essential to help hold the body together, but having too much can cause the body’s tissues to stiffen and thicken.
What are the symptoms of Scleroderma?
Main symptoms of localized scleroderma is thickening of skin which may occur as patch [morphea], linear Scleroderma [ A single line or band of thickened & or abnormally colored skin]. These occur mostly in children.
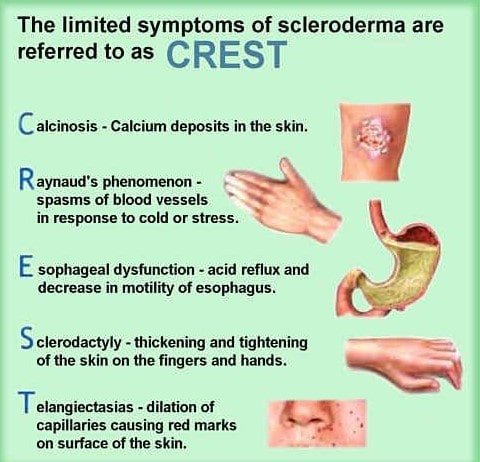
People with limited form of systemic Scleroderma may present with what is commonly called as the ‘CREST’.
C– Calcinosis formation of calcium deposits in the connective tissues.
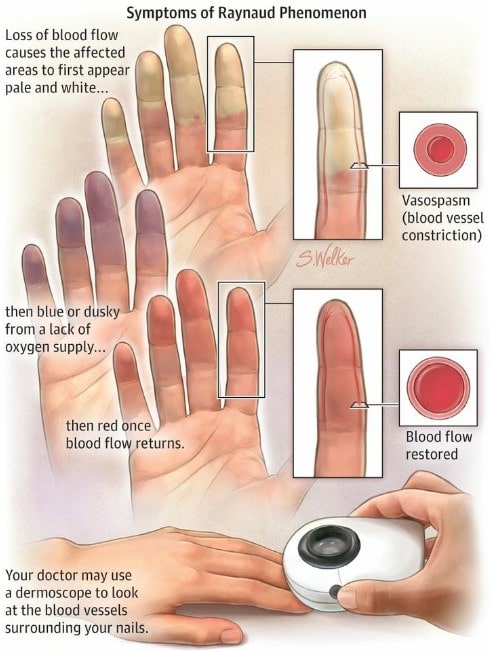
R– Raynaud’s phenomenon a condition where hands or feet turn white & cold, then blue in colour. As blood flow returns they become red.
E– Esophageal dysmotility-impaired function of the tube connecting the throat & the stomach that occurs when smooth muscles in the esophagus lose normal movement.
S– Scerodactyly-thick, tight skin on fingers,
resulting from deposits of excess of collagen in the skin. Skin appears shiny, tight, darkened & makes it hard to bend/straighten fingers.
T-Telangiectasias-small red spots on the hands & face that are caused by swelling of tiny blood vessels. Other symptoms include tiredness, loss of hunger, weight loss, joint swelling & pain. Generalised or diffuse scleroderma and sine scleroderma are other forms of scleroderma.
Systemic sclerosis can cause a range of symptoms affecting many different parts of the body
- Increased sensitivity to the cold
- Joint or muscle pain and stiffness
- Digestive problems
- Changes in the skin
- fingers or toes turning white then blue in the cold
How it is diagnosed?
There’s no single test for systemic sclerosis, and the characteristic thickening of the skin is often the key factor in making the diagnosis. However, tests can be helpful in finding out whether other parts of the body are affected.
Tests could include:
- blood tests
- x-rays and computerised tomography (CT) scans
- breathing tests
- a heart scan (echocardiogram or ECG)
- stomach tests (for example an endoscopy)
What treatments are there?
Ususally a rheumatologist [a specialist who treats people with diseases of joints, bones, muscles and Immune system] treats the case. Other specialists are also involved such as a dermatalogist, nephrologists, cardiologist, gastro-enterologist and pulmonary specialist depending on presentation.
Current treatment is mainly focusing on symptom control and management of organ damage. Thus treatment and management focus on relieving symptoms and limiting damage. Mycophenolate is a good drug for overall disease control including lung disease in Scleroderma.
At the moment there’s no cure for systemic sclerosis, although medications can help to control the symptoms and treat any complications. There’s also a lot you can do for yourself, including exercise and skin care, that will help in managing your condition.
The treatment you’re given will depend on your symptoms. It can include:
- ant acids for heartburn
- pain killers and non-steroidal anti- inflammatory drugs (NSAIDs) for joint pain
- ACE inhibitors for high blood pressure and kidney problems
- steroid tablets or immunosuppressive drugs (usually in more severe cases).
With regular follow ups under a physician, women with Scleroderma can have safe pregnancies & healthy babies. If not supervised by expert, pregnancy & child birth related complication do happen.
